How the Gut and Brain Work Together
Belly butterflies are not just for the stomach anymore. A new study shows that there is actually a connection between gut and mind: IBS, stress, food – your gut affects it all! But science can help by understanding this ‘gut-brain to improve mental health.
The gut-brain axis
The gut-brain axis is a two-way communication system between the brain and belly, so it should come as no surprise that they’re each others’ best friends. The success of this relationship relies on three things: (1) communicating via neurotransmitters to maintain homeostasis; (2) working together towards your well-being; and finally, understanding one another to communicate effectively back and forth.
The guts are ruled by the neurotransmitter serotonin, which plays an important role in mood regulation. Basically, if you’re feeling stressed out or too happy for someone else’s taste, then there may be some signaling imbalance going on down south!
- The brainThe nerves surrounding
- The gut (enteric nervous system)
- The vagus nerve
- Gut bacteria (the microbiome)
- Hormones such as serotonin
What is the Enteric Nervous System?
The gut has 100 million neurons and is called the “second brain.” These enteric nervous systems (ENS) are responsible for controlling motility – which dictates how food moves through your intestines, as well as fluid secretion. The ENS network extends from the esophagus to the anus.
The second brain in your gut is the one that needs to be taken care of if you want a happy mind and body. The vagus nerve sends signals from our head and stomach, so it plays a key role in psychiatric diseases like anxiety and gastrointestinal problems such as diarrhea or constipation.
The oldest part of this ‘second brain’ is called the enteric nervous system (ENS), with 500 million neurons – about twice the number found in the spinal cord!
It’s time to start thinking about your gut. Recent studies have found that abnormal brain-gut communication can lead to various health problems, including depression and anxiety. Disruption in the ENS might be the culprit for these mental illnesses because it has been shown to interfere with our body’s ability to maintain homeostasis–a state where all bodily functions are working together at their most efficient levels during optimal physiological conditions. Interestingly enough, stress or emotional responses can also elicit exaggerated gut reactions such as nausea or diarrhea due mainly to increased intestinal permeability, allowing substances from outside sources into our system without being filtered out by other means (such as stomach acids). These findings show just how important maintaining healthy brain/bowel interactions is if.
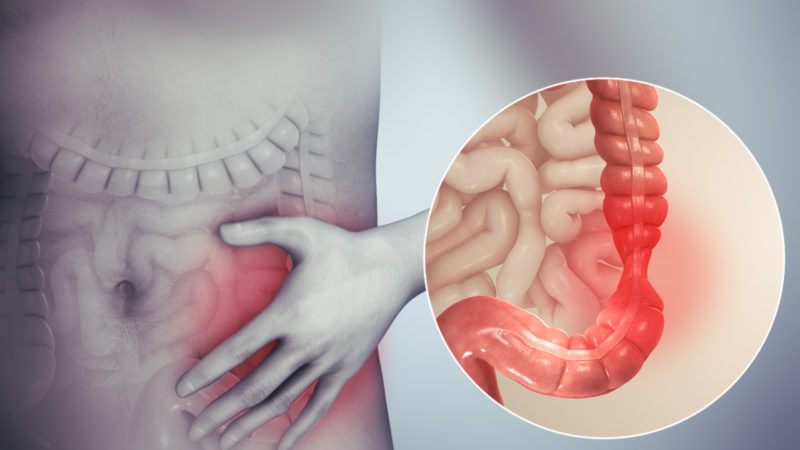
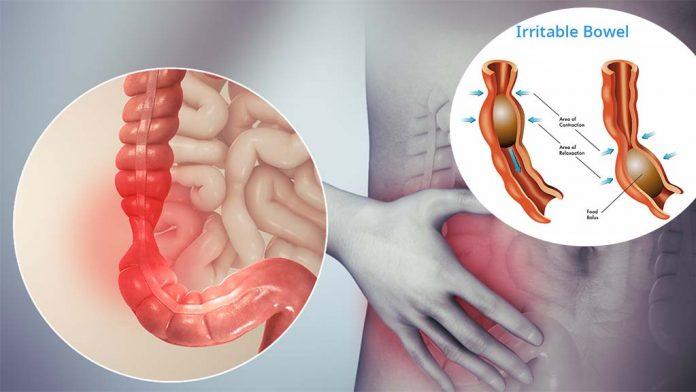
Anxiety and bowel issues
The link between gut and brain explains how stressful situations – such as giving a presentation or sitting an exam – may cause nausea, abdominal pain, anxiety, etc. Stress causes material in the GI tract to pass more quickly, resulting in symptoms of IBS (irritable bowel syndrome). There are several theories about this phenomenon. One suggests stress might have reduced blood flow, leading to increased activity of smooth muscles within your intestines that would then lead to spasms and cramping.
There is also evidence linking structural changes with psychological distress – people who experience high levels of mental anguish often show signs of physical damage on their intestinal lining.
- Heightening sensitivity to pain (visceral hypersensitivity)
- Activating the immune system causing
- inflammationInfluencing microbiota
- Altering motility (the speed of material through the intestines)
Irritable bowel syndrome: gut-brain dysfunction
Gut-brain miscommunications can lead to a variety of diseases, many not yet understood. For example, Irritable Bowel Syndrome (IBS) is the most common disorder arising from gut-brain interactions and affects 1 in 9 people globally. (8). IBS has symptoms including abdominal pain associated with either constipation or diarrhea. Other symptoms include:
A feeling that one’s bowel does not empty after having gone to the bathroom; A sudden change in stool frequency – going more often than usual or less frequently; Clogged rectum – difficulty passing stools due to tightness at the anus.
- Abdominal pain and bloating
- Bloating
- Constipation or diarrhea
- Nausea
- Wind
IBS is both physically and mentally impairing. Several studies have shown the severity of IBS can be worsened by mental health problems, such as depression or anxiety disorder. This goes to show that there’s a clear connection between your gut and how you feel about yourself!
- The link between IBS and psychiatric illnesses such as depression or anxiety can be attributed to the stress of dealing with both at once.
- Patients with Irritable Bowel Syndrome, or IBS, experience an increase in severity of symptoms during times when they are experiencing significant amounts of stress.
Symptoms such as abdominal pain and discomfort exacerbate a person’s emotional state; because the gastrointestinal tract is so closely linked to other areas like mood regulation centers within the brain, there can be close links between how you feel on both sides of your body.
- Psychological therapies such as hypnotherapy, cognitive-behavioral therapy (CBT) and mindfulness meditation have been shown to be helpful for those with IBS.
The ENS: An opportunity for therapy
Many factors go into this connection, and the logic behind it is as follows: The brain controls our mood, appetite, bowel movements, etc. Meanwhile, the ENS aids in these bodily functions by creating balance when we are getting too much or insufficient stimulation from other areas like taste buds. This then leads to us feeling a sense of control over what happens without bodies on both ends, leading to more positive thoughts about ourselves overall, leading to an increased confidence level that affects how others see you outside your body (i.e., mind-body).
The effectiveness of antidepressants and cognitive behavioral therapy techniques such as hypnotherapy have been proven time after time for treating IBS due largely to their ability to affect 2 brains.
When gastroenterologists prescribe antidepressants or psychological treatments after a diagnosis of irritable bowel syndrome, they are not suggesting that the patient is crazy. They do this because there has been researched to show these medications can benefit patients with IBS-D by increasing serotonin and other neurotransmitters in their brains, which also affect ENS neurons in the gut.
When doctors write prescriptions for mood-stabilizing drugs like Prozac and Lexapro following diagnoses of Irritable Bowel Syndrome – Dysmotility Type (IBS-DM), it’s often seen as an indication that symptoms must be all “in your head.” This isn’t accurate, though; rather than just being prescribed blindly without merit, these medicines could actually provide relief from debilitating effects.
Psychological therapies for bowel disorders
- Gut-directed hypnotherapy: You want to improve your symptoms of IBS? This doctor is a specialist in it. With the help from science and hypnosis, you’ll visualize your gut as tubes with fast-flowing contents to make improvements easier!
- Mindfulness meditation: in this practice, based on Buddhist tradition, patients are guided to bring their awareness to the present moment and accept physical sensations as they happen. This has been shown in studies to help improve symptoms of IBS.
- Cognitive-behavioral therapy (CBT): Scientists are looking for a cure to the common stomach disorder IBS. One of their main goals is trying to correct people’s negative thoughts about symptoms and relive some of the pain caused by irritable bowel syndrome.
The gut affects the brain, too
Not only does your gut affect the brain, but it can also influence how healthy you are. For example, if there is an imbalance of bacteria in your intestines, this could lead to conditions like autism or schizophrenia without any warning signs beforehand.
The microbiome
The trillions of microbes living in the GI tract, collectively known as the microbiome, provide a fascinating glimpse into how we digest food. When consuming fiber, these microscopic organisms produce short-chain fatty acids that can affect our brain function. This is because many of these compounds are neuroactive, and they cross over to the central nervous system from blood vessels via tight junctions between cells called gap junction channels (or connexons).
When humans eat foods with indigestible fibers like cellulose or hemicellulose, their bodies will not extract all necessary nutrients from this type of digestion alone; however, some gut bacteria species may help break down certain plant materials for energy production. The process by which plants capture sunlight through photos.
With an oversupply of harmful bacteria in the gut, one may experience inflammation and depression. Probiotics can help to reduce this by preventing inflammatory signals from being released into the body.